Surgical treatment for lymphedema
Surgical techniques for lymphedema have progressed considerably in recent years. The goal of these procedures is to improve lymphedema, even if it cannot be cured.
The benefits of lymphedema surgery can be:
- Decreased arm / leg perimeter, favoring the return of lymphatic fluid (less swelling).
- Decrease in the number of infections.
- Decreased pain and / or feeling of heaviness.
In addition to surgical treatment of lymphedema, non-surgical treatment must be continued (compression garments, manual lymphatic drainage, etc.).
Surgical techniques for lymphedema
1.- Lymphovenous Anastomosis (LVA)
Lymphatic vessels are connected to the venous system to facilitate drainage of the lymphatic fluid. Lymph can be diverted into the bloodstream to decongest the affected limb.
DURATION OF SURGERY
The duration of this procedure depends on the number of anastomoses that can be performed. It usually takes between 1 and 4 hours.
SURGICAL TECHNIQUE
Small incisions are made in the arm or leg. A superficial vein (venule) and the lymphatic vessel are located by injecting the indocyanine green dye.
Both vessels are connected by microsurgery techniques – a high-magnification microscope and very fine surgical suture (thread) are required. Subsequently, the skin incisions are sutured, and a soft dressing is applied.
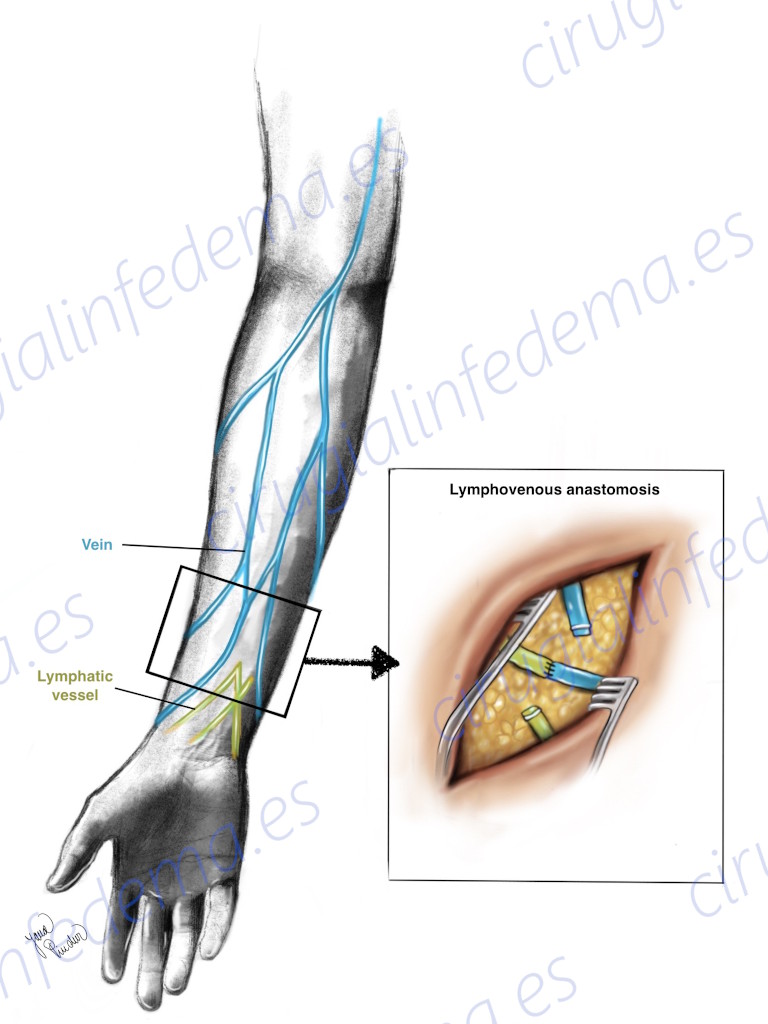
Surgical Technique of Lymphovenous Anastomosis
After opening the skin, a lymphatic vessel and a small vein are identified, which are connected to each other. Thus, stagnant lymph is diverted into the bloodstream.
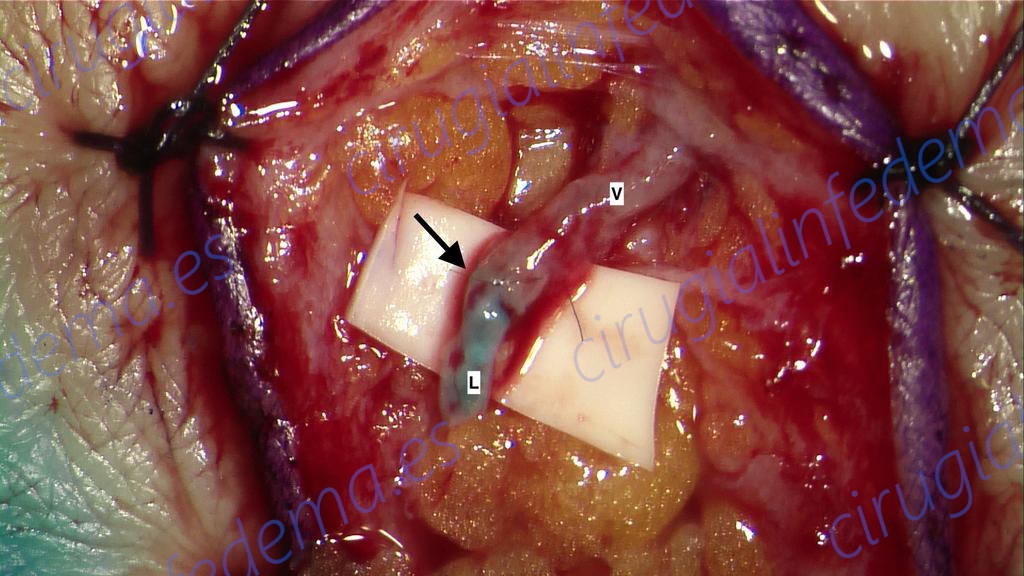
Example of Lymphovenous Anastomosis
The lymphatic vessel (marked with the letter “L”) is connected to a vein (marked with the letter “V”). The arrow indicates the area of connection between the both structures (anastomosis).
ADMISSION TO HOSPITAL
Outpatient setting (does not require hospital admission).
POSTOPERATIVE
Upon discharge you will be able to walk and live a relatively normal life, avoiding exercise during the first 6 weeks. The sutures (stitches) on the skin are removed after 2 weeks.
After surgery, you should wear a lightly compressive bandage on the operated limb.
After the 5th week, you should start manual lymphatic drainage and wear compression garments. Sun protection is essential at least for the first year.
2.- Lymph Node Transfer (LNT)
It consists of obtaining lymph nodes from another location and transplanting them to the affected area.
The goal of this surgery is double: the new lymph nodes produce growth factors that allow the formation of new lymphatic vessels and absorb lymph; on the other hand, this new transplanted tissue decreases the scar in the affected area.
Scientific studies have observed that results can take up to a year to appear.
DURATION OF SURGERY
The duration of this intervention is usually 4-5 hours.
SURGICAL TECHNIQUE
Donor lymph nodes are removed with an artery and a vein. They are then placed in the affected area (armpit or groin), and the artery and vein of the lymph nodes are connected to another artery and vein in the recipient area using microsurgery techniques – under high magnification microscope and very fine surgical suture (thread).
DONOR AREA OF LYMPH NODES
There are different areas from which lymph nodes can be obtained. It is important to make a correct selection, to avoid the appearance of lymphedema in the donor area. We generally use lymph nodes from the supraclavicular region.
There are other donor areas, such as the inguinal area. These nodes are commonly used at the same time of breast reconstruction, when the latter is performed with the patient’s own tissues obtained from the abdomen (DIEP flap).
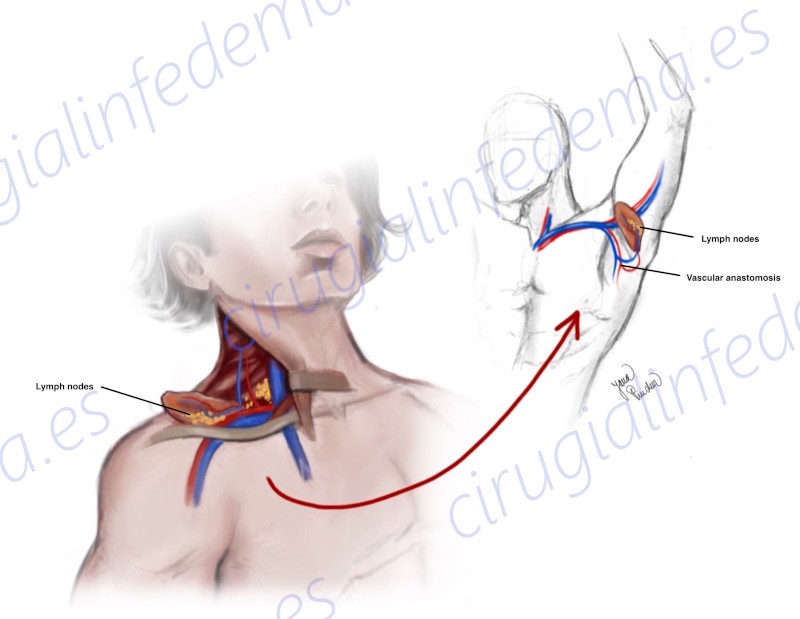
Surgical Technique of Lymph Node Transfer
The ‘donor’ lymph nodes of a healthy area with their blood vessels are located and transplanted to the area of damaged nodes (armpit or groin).
ADMISSION TO HOSPITAL
3-7 days.
POSTOPERATIVE
Upon discharge you will be able to walk and live a relatively normal life, avoiding exercise during the first 6 weeks.
The sutures (stitches) on the skin are removed after 2 weeks. After surgery, you should wear a lightly compressive bandage on the operated limb and start manual lymphatic drainage.
You should avoid the massage on the lymph node transfer (armpit or groin). Sun protection is essential at least for the first year.
3.- Liposuction
Liposuction of the affected limb consists of absorbing the lymphatic fluid and some excess fatty deposits through a cannula.
This procedure, unlike lymphatic-venous anastomoses and lymph node transplantation, is considered “non-physiological”: it does not spontaneously improve lymphatic drainage, but rather it performs drainage without improving the lymphatic system.
Compression garments must be worn after any surgical procedure. However, it is especially important after liposuction, to avoid an increase of fluid in the limb and to allow the skin to readjust.
DURATION OF SURGERY
2-3 hours.
SURGICAL TECHNIQUE
The suction cannula is inserted through small incisions in the arm or leg. A superficial aspiration of the lymphatic fluid is performed. Sometimes, it is convenient to combine it with the marking of the lymphatic vessels with indocyanine green to avoid damaging them.
ADMISSION TO HOSPITAL
Outpatient setting (does not require admission).
POSTOPERATIVE
Upon discharge you will be able to walk and live a relatively normal life, avoiding exercise during the first 6 weeks. The sutures (stitches) on the skin are removed after 2 weeks. After surgery, you should wear a compression garment. Bruises are common, which will disappear after a few days. Sun protection is essential at least for the first year.
4.- What surgical technique is suitable for me?
The choice of surgical treatment must be personalized. It is important that a team with experience in lymphedema assess your case and decide which is the most suitable procedure for you.
We can generalize the following principles:
- The above surgical techniques can be combined to achieve the best result.
- Physiological surgical techniques (lymphovenous anastomosis and lymph node transfer) must be performed before liposuction. In our experience, liposuction should be used as the last resource or for severe cases.
- For lymph node transfer: The greater the scar in the armpit or groin, the better results will be obtained (associated with scar removal in that area). Patients who have undergone breast cancer treatment with radiation therapy, and who have a lot of scar in the armpit area, are good candidates for this procedure.
- When visualizing “clogged” lymphatic vessels with the indocyanine green technique, the best results are obtained with the lymphovenous anastomosis. In contrast, if lymphedema is more severe and there is absence of lymphatic vessels, this technique cannot be performed.